

What is percutaneous discectomy?
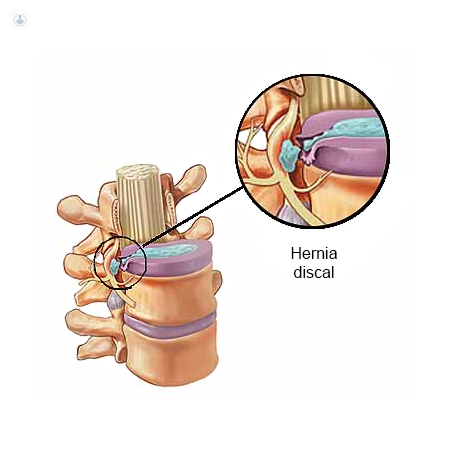
Percutaneous discectomy surgery is a minimally-invasive technique used to treat herniated discs in the spinal column, in the lumbar region as well as the cervical region, without the need for open surgery.
Why is it done?
Disc herniation is a frequent condition that in many cases is incapacitating, sometimes so much so that rest and rehabilitation are not sufficient and surgery becomes necessary.
Medical advancements have led to the availability of minimally-invasive techniques, such as percutaneous surgery, which offer greater advantages:
- Small incisions are made to repair the damaged section.
- Wounds in the skin and muscles are minimal.
- Post-operative recovery is much shorter and less painful.
What does percutaneous discectomy involve?
The surgery involves extracting the pulpous nucleus of the intervertebral disc via a small incision in the skin. This is done with the aid of an endoscope, a slim tube fitted with a lens that enables visualisation of structures and tissues on a screen, and fine instruments such as a laser and a radiofrequency probe.
How to prepare for percutaneous discectomy:
Before surgery, it is advisable to try and achieve the best physical condition possible, via measures such as:
- Eating well: Good nutrition is key to maintaining a healthy immune system. In the weeks before the operation, eat a balanced diet and take vitamin supplements. This will help to reduce the risk of infection.
- Get fit: Weak muscles and low cardiovascular fitness make post-surgical recovery more difficult.
- Do not smoke. Patients who stop smoking are more likely to have a successful surgery.
Care following percutaneous discectomy surgery:
You can return home the same day as the procedure and can resume your normal routine within 3-5 days after surgery.
Alternatives to percutaneous discectomy surgery for treating herniated discs:
- Ozone therapy: There are several techniques for applying ozone locally to the herniated disc, but the most effective and commonly used is paravertebral injection. Its primary advantage versus other techniques is its efficacy: it has a 90% success rate, as it is an outpatient treatment with few side-effects and is very well tolerated by patients.
- Orthokine therapy: In this technique, proteins and growth factors obtained from the patient’s own blood are injected into the affected area. The blood is extracted with syringes, incubated and centrifuged to yield a blood serum that is then reinjected into the joint.
