

What is cirrhosis?
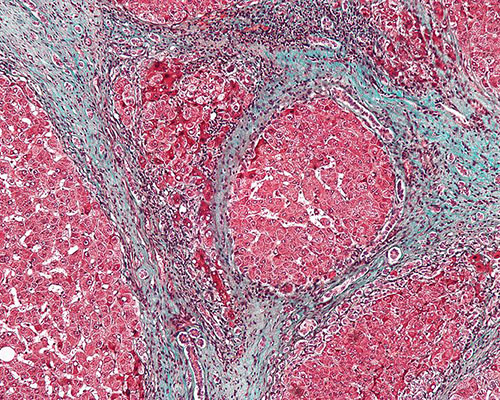
Cirrhosis is a disease in which the liver gradually deteriorates due to chronic injury and scarring which results from a variety of factors. The liver has the ability to repair itself, so each time the organ is injured, scar tissue is formed during the healing process. As cirrhosis progresses, more scar tissue is formed, partially blocking blood flow through the liver.
In general, liver damage caused by cirrhosis is irreparable, although early diagnosis of cirrhosis can limit or even reverse the damage.
There are different types of cirrhosis:
- Alcohol-related cirrhosis: this is caused by excessive alcohol consumption and is the most common cause of cirrhosis
- Hepatitis-related cirrhosis: this is caused by the hepatitis virus, making the liver inflamed
- Cryptogenic cirrhosis: it is referred to as this when the cause for the cirrhosis is unknown
- Primary biliary cirrhosis: the immune system causes cirrhosis by mistakenly attacking healthy liver cells, which are subsequently replaced by scar tissue
- Secondary biliary cirrhosis: causes blockage of the bile ducts
- Sclerosing cirrhosis: the bile duct narrows, preventing the bile from flowing out.
Prognosis of cirrhosis:
Cirrhosis is an incurable disease which, if it progresses without a correct diagnosis, can lead to serious complications such as:
- Portal hypertension: high blood pressure in the veins of the liver. Blood flow is reduced, which increases the pressure in the vein that carries blood from the intestine to the liver.
- Swelling in the legs and abdomen: portal hypertension can lead to oedema and ascites, i.e. fluid formation in the legs and abdomen respectively. Both conditions may also be due to the liver's inability to generate the necessary amount of protein in the blood.
- Splenomegaly: an enlarged spleen. A decrease in the number of white blood cells and platelets in the blood may be a sign of cirrhosis.
- Bleeding: portal hypertension can cause the blood to flow into small veins, causing them to increase in size and possibly rupture, leading to severe bleeding. This bleeding is potentially fatal if the veins in the lower oesophagus (oesophageal varices) or stomach (gastric varices) rupture.
Other complications include:
- Jaundice: the skin becomes yellow due to the inability of the liver to remove bilirubin.
- Malnutrition: cirrhosis can hinder the absorption of nutrients, leading to weakness and weight loss
- Infections: cirrhosis reduces the body’s ability to fight infections
- Hepatic encephalopathy: an accumulation of toxins in the brain, which can cause mental confusion
- Osteoporosis: in some cases, people with cirrhosis lose bone strength and are more prone to factures
- Increased risk of liver cancer
- Acute or chronic liver failure
Symptoms of cirrhosis:
One of the main problems with cirrhosis is that there are often no signs or symptoms until the disease is quite advanced and liver damage is significant. Some of the most common symptoms of this disease are:
- Tiredness
- Bleeding easily
- Itchy skin
- Jaundice
- Ascites
- Bruising easily
- Loss or lack of appetite
- Low sex drive
- Nausea
- Swelling in the legs
- Drowsiness
- Weight loss
Can cirrhosis be prevented?
The best way to prevent cirrhosis is to take care of your liver. Therefore, you should:
- Avoid drinking excessive amounts of alcohol
- Eat a healthy, balanced diet
- Maintain a healthy weight
- Reduce your risk of getting hepatitis by having protected sex and not using illicit drugs, particularly those that are injected. There is also a vaccine now available for hepatitis B.
Treatments for cirrhosis:
Treatment for cirrhosis will vary depending on the cause of the disease and whether other complications are present. The aim of treatment is to slow the progression of scar tissue in the liver. In the event of complications, hospitalisation may be necessary. The main treatments are:
- Eating a nutritious diet
- Avoiding alcohol and other substances that can affect liver function
- Diuretics are recommended for oedema and ascites
- Beta-blockers that lower blood pressure may be prescribed for portal hypertension
- Hepatic encephalopathy is treated by cleansing the intestine with lactulose
- People with cirrhosis and hepato-renal insufficiency should have haemodialysis
- Liver transplant. In advanced cases of cirrhosis where the liver stops working, liver transplantation may be the only option. With transplantation, the diseased liver is replaced with a healthy liver from a deceased donor, or with part of the liver of a living donor.
Which specialist treats cirrhosis?
The specialist who diagnoses and treats cirrhosis are hepatologists.
